
The management of narcolepsy involves non-pharmacological and pharmacological approaches with an increasing number of symptomatic treatment options for adults and children that have been studied in some detail. Treatment choices should be tailored to each patient’s symptoms, comorbidities, tolerance and risk of potential drug interactions. The main recommendations can be summarized as follows: (i) excessive daytime sleepiness in adults-scheduled naps, modafinil, pitolisant, sodium oxybate (SXB), solriamfetol (all strong), methylphenidate, amphetamine derivates (both weak) (ii) cataplexy in adults-SXB, venlafaxine, clomipramine (all strong) and pitolisant (weak) (iii) excessive daytime sleepiness in children-scheduled naps, SXB (both strong), modafinil, methylphenidate, pitolisant, amphetamine derivates (all weak) (iv) cataplexy in children-SXB (strong), antidepressants (weak). ResultsĪ total of 10,247 references were evaluated, 308 studies were assessed and 155 finally included. Following a systematic review of the literature (performed in Fall 2018 and updated in July 2020) recommendations were developed according to the GRADE approach.

According to the EAN recommendations, 10 relevant clinical questions were formulated in PICO format.
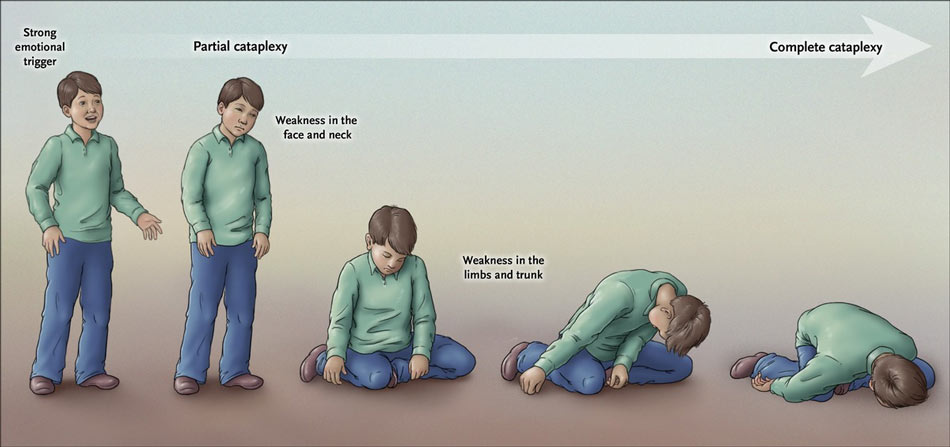
The European Academy of Neurology (EAN), European Sleep Research Society (ESRS) and European Narcolepsy Network (EU-NN) nominated a task force of 18 narcolepsy specialists. This paper aims to provide evidence-based guidelines for the management of narcolepsy in both adults and children. Sleep Medicine.Narcolepsy is an uncommon hypothalamic disorder of presumed autoimmune origin that usually requires lifelong treatment. The clinical features of cataplexy: A questionnaire study in narcolepsy patients with and without hypocretin-1 deficiency. van NU SJ, van der Zande WL, Donjacour CE, van Mierlo P, Jan Lammers G.To reduce the symptoms of narcolepsy, including cataplexy and drowsiness, scheduling short daytime naps and maintaining healthy sleep habits is recommended. In this sense, the interventions are focused on the prevention of these episodes from the identification of symptoms that precede them: learning to detect prodrome of cataplexy is useful to be able to react to them when they begin to occur in the future. Psychology can also contribute to the treatment of cataplexy. Other drugs that are used in cases of cataplexy and narcolepsy in general are stimulants, such as modafinil, and antidepressants, particularly tricyclics and venlafaxine, a selective serotonin and norepinephrine reuptake inhibitor. Gammahydroxybutyrate has similar effects. The treatment of choice is sodium oxybate, a very safe drug that is also effective in fighting daytime sleepiness. Treatment and preventionĬataplexy it is mainly treated by drugs.

In this sense, many experts consider narcolepsy an autoimmune disorder related to the so-called “human leukocyte antigens” (HLA).

In many cases narcolepsy and cataplexy have a genetic component. Damage to the hypothalamus, which secretes hypocretin, is frequently involved in the development of this disorder. In this way, These episodes can occur as a result of brain injuries, malformations and tumors.īrain infections, vascular accidents, or diseases such as multiple sclerosis can also cause episodes of cataplexy. Specifically, it is believed that cataplexy episodes are the consequence of sudden and generalized inhibition of motor neurons at the level of the spinal cord, which causes a loss of muscle control.Īny alteration that reduces orexin levels is likely to cause narcoleptic symptoms such as cataplexy. Orexin plays a fundamental role in maintaining wakefulness and alertness its deficit has been related to REM intrusions typical of narcolepsy. The main cause of narcolepsy and cataplexy is considered to be the presence of low levels of the hormone orexin or hypocretin in the cerebrospinal fluid. Other symptoms that occur regularly during cataplexy episodes are pronunciation difficulties and visual disturbances, particularly blurred or double vision.


 0 kommentar(er)
0 kommentar(er)
